
Disease Areas: Addiction
Addiction
We have been at the forefront of addiction medicine for almost two decades, seeking to help people living with alcohol dependence and people living with opioid dependence along their recovery journeys. Beyond our commitment to develop medicines, we seek to raise awareness of the issues experienced by people living with addiction and advocate for increased access to treatment for these chronic diseases. We are steadfast in our belief that addiction is a public health crisis, not a moral failing, and, as with other chronic illnesses, treatment is available and may help.
Evolving Terminology
The terminology used to describe problematic alcohol and opioid consumption has changed over time. The historical term “addiction” is now described as “substance use disorders” characterized by a severity range of mild, moderate to severe. These modern terms replaced the previous diagnostic categories of “dependence” (problematic use with physical dependence) and “abuse” (problematic use without physical dependence) in previous literature. Below, we use the terms alcohol use disorder (AUD) and opioid use disorder (OUD), which is consistent with the current literature.
Alcohol Use Disorder
AUD is characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences.1 It is diagnosed using criteria outlined in DSM-5. Excessive alcohol use is responsible for about 178,000 annual deaths in the United States2 and can cause heart disease, high blood pressure, liver disease and more. As of 2023, access to treatment was not widespread: less than 8% of adults who had alcohol use disorder received treatment in the prior year.3
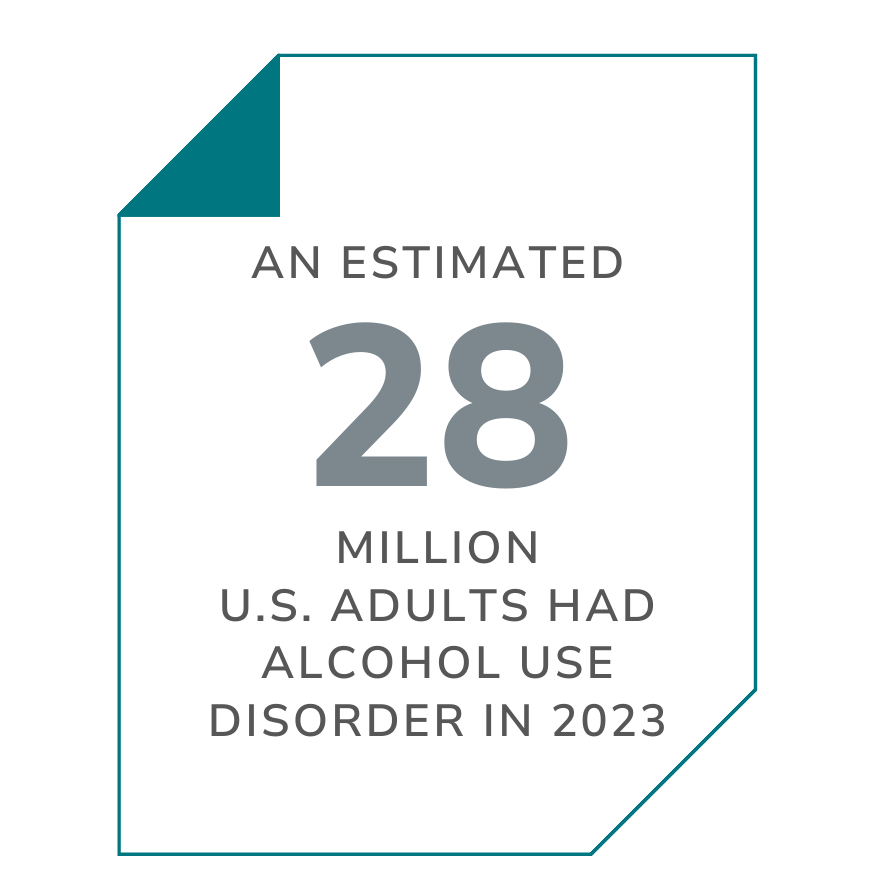 SOURCE: SAMHSA
SOURCE: SAMHSA
Opioid Use Disorder
OUD is a chronic disease characterized by a pattern of opioid use that leads to problems or distress. It is diagnosed using criteria outlined in DSM-5. Representing one of the most pressing public health issues facing our society, opioid overdoses have claimed the lives of more than 320,000 people in the United States since 20175, and OUD cost the United States more than $1.5 trillion in 2020 in total direct and indirect costs.6 Despite the high economic and health burdens of OUD and availability of evidence-based treatment, including FDA-approved medications, treatment remains underutilized. In 2021, only 1 in 5 adults living with OUD received treatment.7
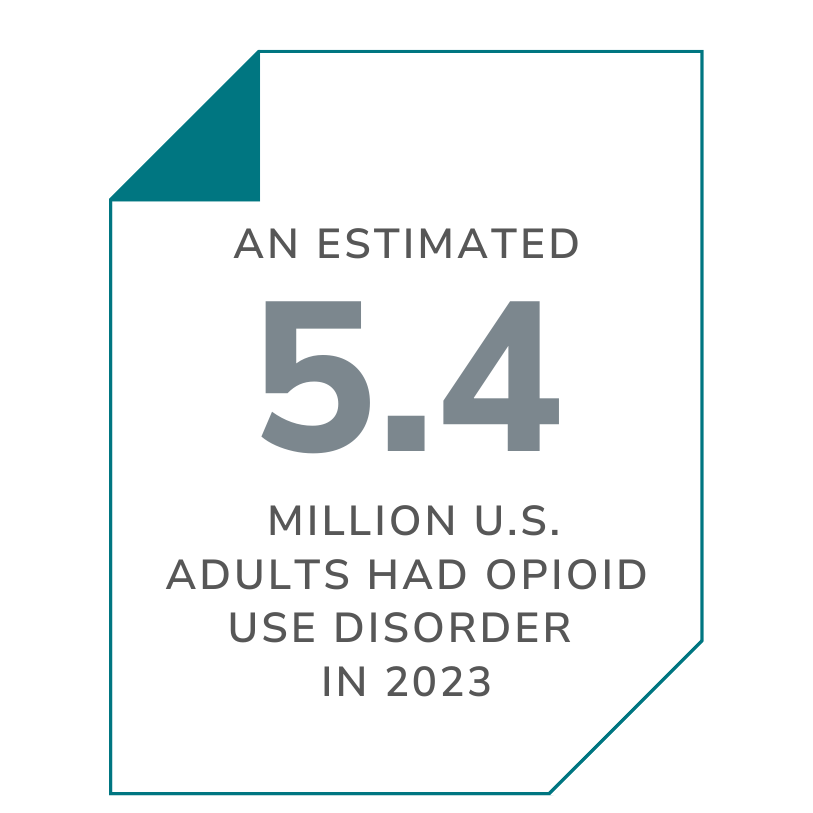 SOURCE: SAMHSA
SOURCE: SAMHSA
Additional Resources
If you’re interested in learning more, below is a partial list of advocacy organizations and resources that can offer additional information on alcohol and opioid dependence.
These links are provided for informational purposes only; they do not constitute an endorsement by Alkermes. Alkermes is not responsible for the content of these third-party sites.



Watching a loved one struggle with drugs or alcohol is heartbreaking and can feel overwhelming but it is essential to remember that recovery is possible. Help is out there and you are not alone.
Ann Herbst,
Executive Director, Young People in Recovery
